Report on the James IV Travelling Fellowship
David R. Urbach, MD
Imperial College London
I began my James IV travels in the United Kingdom at Imperial College London, Department of Biosurgery & Surgical Technology, in St Mary’s Hospital, Paddington. This Department, led by Professor the Lord Ara Darzi of Denham, is impressive: a large, exciting, innovative, and productive research unit, filled with some of the brightest, creative and most energetic researchers, clinical fellows, and young faculty that I have seen in all my travels in departments of surgery.

I began with an introduction to the Department, presented by Myutan Kulendran, a graduate student, and Karen Kerr. Karen functions as the director of research operations of the Department, supervising the direction, coordination and rigor of the academic activities, and working with members to develop and fund their projects. Professor Darzi’s vision is evident throughout this Department. Touring through the various research, education, simulation and clinical areas is probably best understood as exploring a physical rendering of the "homunculus" of Professor Darzi’s brain, a tangible realization of his vision of some of the most intriguing and exiting innovations in modern surgery.
Behind each door in the hallways of the Department of Biosurgery & Surgical Technology is something completely different, and you really have no idea what’s behind a door until you open it and walk inside. Is it a conventional research area with study carrels and graduate students? A laboratory with nuclear magnetic resonance and flow spectrometer analyzing cautery smoke effluent? A simulated operating room? Boardroom for policy discussions? A low-cost, deployable OR simulation environment for resource-poor settings?
I began the first day of my visit with "Virtual Worlds and Medical Media", an applied research program led by David Taylor (with Michael Taylor, a student) using  computer based simulation for health and hospital-based applications. They work primarily using the program "Second Life", creating hospital and ambulatory clinic environments that can be toured virtually, and tested for human factors and usability characteristics. They showed me an interesting example of their work in developing a chemotherapy satellite clinic for Memorial Sloan Kettering in New York, as well as creation of new hospital environments that attempt to better integrate primary care with hospital-based care, which historically has been treated quite differently in the National Health Service and way the Trusts are organized.
computer based simulation for health and hospital-based applications. They work primarily using the program "Second Life", creating hospital and ambulatory clinic environments that can be toured virtually, and tested for human factors and usability characteristics. They showed me an interesting example of their work in developing a chemotherapy satellite clinic for Memorial Sloan Kettering in New York, as well as creation of new hospital environments that attempt to better integrate primary care with hospital-based care, which historically has been treated quite differently in the National Health Service and way the Trusts are organized.

Next, down the hall to another door, behind which was Laura Muirhead, a clinical research fellow, and a wet laboratory with heavy equipment including NMR and flow spectroscopy machines. In this lab, study "Metabonomics", she focuses on the analysis of smoke effluent of surgical diathermy. Already, the lab has been able to make major progress in distinguishing factors such as tissue types. Ultimately, this type of analysis could distinguish whether or not a surgeon is cauterizing through a tissue margin involved with tumor, test whether a tissue sample consists of benign or malignant tissue, or provide information about the tissue type. The concept of point-of-care, real-time surgical diagnostics is a major theme of the department. The challenges remaining to be solved include modifying and miniaturizing equipment so it can be effectively used in an operating room environment, better characterization of tissue types based on cautery effluent analysis, and reducing the time required for these analyses to make the technique more useful at the point of care.
Next, I moved to the Paterson Centre, a building that houses active clinical units (clinic, operating rooms, and surgical wards) with research space. The theme of integrating clinical care and research in the same physical space was another major theme of the Department. In the research floor, Zinah Sorefan and Matt Gold showed me the Distributed Simulation environment. Experience from theater make-up and prop skills are clearly an asset here. A low-cost, highly portable, and realistic looking OR simulation environment could be constructed and taken down in about 10 minutes. The distributed simulation focused on the key aspects required for simulation, focusing on features highly relevant to the content of the simulation (eg patient, monitors) and using low-cost props for features that are more peripheral to the exercise.
I next toured through a variety of simulation-based areas, including a Virtual Reality Laboratory (Pritam Singh), and OR Camp (Anisha Perera). These surgical simulation areas had all the retail off-the shelf simulators (VR trainers, MIST VR, Symbionix) as well as some simulators developed in-house.

Phil Pucher, a clinical research fellow, led me through a tour of the Simulated Ward. This research space contains a physical simulation of a real hospital ward environment (in fact, the Distributed Simulation Environment had been constructed there just 10 minutes before, and disappeared by the time we returned to this room!). Innovation in all aspects of surgical care—pre- operative, operative, and post-operative—is another key theme of the Department of Biosurgery & Surgical Technology. Phil reviewed some results of some recent research he had conducted looking at the quality and outcomes of clinical surgical ward rounds. He evaluated the content of these rounds (information collected from history, physical examination, and charts) as well as assessment of non-technical skills of the surgical team.
Initially, the project Phil described seemed very familiar to me, but I didn’t realize the source of my dèja- vu. After a few minutes, though, I realized that I had been a discussant for that very paper that Phil had presented just two weeks before at a Surgical Forum Session at the American College of Surgeons meeting in Washington, DC!
Archie Hughes-Hallett and Philip Pratt demonstrated the Microbot Surgical Suite and Sensing Laboratory, including the "anatomage table". Archie demonstrated the incredible advances made in three-dimensional imaging, image reconstruction, and image rendering and manipulation, all seeking to better integrate three-dimensional imaging into surgical procedures. Technologies allow the visual representation of deep tissue characteristics, helping to localize a tumor (for example, a renal cell carcinoma case that Archie, a urology registrar, demonstrated to me).

I had lunch with Karen Kerr and members of the health policy team (Oliver Keown and Steve Beales) at the Frontline Restaurant just down the street. We had a fascinating conversation about new plans within the Department, including a new academic-industry partnership core to be built in a courtyard area at St. Mary’s hospital, to identify and incubate high-risk/high- reward projects that have the potential to impact health care around the world. I learned about the global summits of health care organized by the department, which focus on the key policy challenges facing health care decision makers and planners around the world.
In the afternoon, I returned to the 10th Floor Policy Boardroom of the Queen Elizabeth Queen Mother Building. Hutan Ashrafian presented to me some of the innovative work he has been doing in the area of bariatric surgery. In his talk "Beneficial Mechanisms of Bariatric Surgery", he reviewed many of the current hypotheses of the metabolic, nutritional and other physiological aspects of bariatric surgery. Hutan’s work in understanding mechanisms of weight loss in bariatric surgery is masterful. I enjoyed on of his very descriptive slides outlining the evolution of bariatric procedures, including all the false-starts and dead ends over the years. The history of innovation in weight loss surgery undoubtedly has many lessons for future development in this area.

At the end of the day, I presented my talk, entitled "What can be learned from non-randomised studies of surgical procedures?" Despite the lateness of the hour (17:00 on Monday), I was speaking to a full room of over 30 students, clinical fellows, and faculty. At the end of my presentation, I was asked several very insightful and thoughtful questions.
My second day at Imperial College began with meeting Elaine Burns and Anne Marie, one of her graduate students. Elaine is a colorectal surgery trainee focusing on Outcome Research in Surgery. She showed me some of her published and current research projects, looking at phenomena such as adverse event reporting and measuring quality, safety and avoidable mortality. We had a long discussion about some of the new and exciting areas in surgical outcomes research, including research on failure to rescue, how this is defined, and the implications for study.

After lunch with Karen Kerr and Elaine Burns, I headed over to the Hamlyn Centre, in the South Kensington Campus of Imperial College. The Hamlyn Centre focuses on surgical robotic technologies. Professor Guang-Zhong Yang is the lead engineer who has led the majority of the projects from the technical and engineering side. I toured a showpiece museum of surgical robotics, including working surgical robots as well as informative and professional
video presentations. Some of the new technologies being developed by the engineers are really exciting. In one room, I saw a demonstration of miniature three- dimensional portable accelerometers (worn over the
ear) that can be used to quantify the quality and quantity of movement, for example in patients rehabilitating
from orthopedic surgery. The potential for measurement of post-operative recovery in surgical patients is another exciting research opportunity. There are a number of 3-D printers that
are used to provide rapid prototypes of newly designed and engineered devices, and machines to
 manufacture engineered products for robotics. Another new and exciting concept is a visual-field tracking mechanism that can guide surgical robots, essentially forcing the robotic arm to move a camera or instrument to move in the direction of an operator’s gaze, as measured by eye-movement tracking.
manufacture engineered products for robotics. Another new and exciting concept is a visual-field tracking mechanism that can guide surgical robots, essentially forcing the robotic arm to move a camera or instrument to move in the direction of an operator’s gaze, as measured by eye-movement tracking.
I concluded my tour of Imperial College London with a visit to the Paterson Centre. Mr. Barry Paraskeva, Chief of Surgery, led me on a tour of the building. Once again, I was impressed by the physical proximity of research laboratories and creative spaces with real working clinical care environments. The clinical operations in the Paterson Centre are designed to maximize efficiency, ensuring close proximity of pre- operative, operative, and post-operative clinical areas, and smooth patient flow and transitions between units. I toured the theatres, where colorectal procedures and laparoscopic cholecystectomy were being performed.
University of Edinburgh
My host in Edinburgh was O James Garden, Regius Professor of Clinical Surgery and Honorary Consultant Surgeon. Professor Garden trained in Edinburgh, Glasgow and Paris from 1978 to 1988, as Chef de Clinique in the unit of Professor Henri Bismuth in hepatobiliary and liver transplant surgery. Professor Garden holds a number of international leadership positions in surgery, including President of IHPBA, Chairman of the British Journal of Surgery Society, Director of Surgical Distance Learning - Edinburgh Surgical Sciences Qualification (MSc Surgical Sciences, ChM in General Surgery), Member of Council of the Royal College of Surgeons of Edinburgh, Honorary Secretary of the James IV Association of Surgeons, and Editor-in-Chief of HPB.
We began my first day in Edinburgh with a fascinating tour of its surgical history, led by the premier guide to Scottish surgical tradition, Professor Garden. We surveyed the old Victorian-era construction of the Royal Infirmary of Edinburgh buildings, used as a functioning hospital until only a few years ago when the RIE moved to its new premises. This hospital was the center of complex surgery in Edinburgh, with operating rooms and Nightingale-style nursing wards functioning in a centuries-old structure. We visited the University of Edinburgh, with its buildings steeped in surgical tradition.
Next we drove to the University of Edinburgh, past the old Anatomy Department where Professor Robert Knox worked as a renowned anatomy lecturer in the 19th century. Edinburgh’s rich surgical history is checkered by intriguing and peculiar characters, one of which was definitely Robert Knox. Knox’s career was ruined by the macabre "Burke and Hare" case. William Burke and William Hare discovered the value of corpses to Knox’s Anatomy Department, always in search of dissection material for teaching anatomy to the medical students. After accidentally discovering a dead body and selling it to Dr. Knox for a tidy profit, the two entrepreneurial conspirators solved the problem of their lack of cadavers for sale, by murdering the wretched poor living in the streets of Edinburgh. After murdering over a dozen people and selling their bodies to Knox, the two were caught. Hare was convinced to testify against Burke in court, who was hanged for the crimes.

Knox was never punished for his part in the business, which apparently angered the people off Edinburgh. Knox was harassed by the people and censured by the Royal College of Surgeons of Edinburgh, losing his prominent role in Edinburgh.
We did a quick tour of some of the University of Edinburgh buildings, including the neo-classical Playfair Library Hall, designed by William Henry Playfair, one of the great Scottish architects. William Henry Playfair was the nephew of the Scottish philosopher and mathematician John Playfair.
We next drove to the magnificent headquarters of the Royal College of Physicians of Edinburgh, now over 500 years old. Here were portraits of great surgeons, including Joseph Bell, who was a president of the Royal College of Surgeons of Edinburgh and personal physician to Queen Victoria when she visited Scotland. Bell was renowned for his excellent diagnostic skills, advocating close observation of patients to make a correct diagnosis. He would demonstrate his powers of observation to students by selecting a stranger, and guess his occupation or recent activities based solely on close observation. One of Bell’s clerks was Arthur Conan Doyle, the Scottish physician and creator of Sherlock Holmes. Conan Doyle credited Bell as the inspiration for the fictional detective Sherlock Holmes.

Among the portraits in the College building was King James IV, considered a "renaissance" king, whose interest in science led to the incorporation of the Royal College of Surgeons of Edinburg in 1506. A portrait of Joseph Lister dominates the Fellows Room. Lister popularized the concept of antisepsis in surgery at the Glasgow Royal Infirmary. He used carbolic acid to sterilize surgical instruments and to disinfect wounds. At the Royal Infirmary of Edinburgh, Lister worked with the surgeon James Syme.

Another notable portrait was John Bruce, founder of the James IV Association of Surgeons. In 1956 he was appointed Regius Professor of Surgery at Edinburgh University. He was editor of the Journal of the Royal College of Surgeons of Edinburgh. Bruce was knighted in 1963, and served as President of the Royal College of Surgeons of Edinburgh from 1957-1962.
After the tour of the Royal College of Surgeons of Edinburgh, Professor Garden
drove me to the new Royal Infirmary of Edinburgh hospitals. Much more modern than the old premises, the building was partitioned between the University areas and the hospital. I first met with Professor
 Stephen Wigmore, Professor of Transplantation Surgery and Honorary Consultant Surgeon, and a previous James IV traveller. Professor Wigmore is head of Hepatobiliary-Pancreatic Surgical Services and Edinburgh Transplant Unit, Royal Infirmary of Edinburgh. His clinical interests lie in liver transplantation and hepatobiliary surgery. His principal research focus is on the cell and molecular biology of organ pre-conditioning and stress protein expression. Other research interests include the Kupffer cell, innate immunity, endotoxin handling and functional assessment of the liver in the context of surgery and transplantation. He is also involved in medical education and
distance learning.
Stephen Wigmore, Professor of Transplantation Surgery and Honorary Consultant Surgeon, and a previous James IV traveller. Professor Wigmore is head of Hepatobiliary-Pancreatic Surgical Services and Edinburgh Transplant Unit, Royal Infirmary of Edinburgh. His clinical interests lie in liver transplantation and hepatobiliary surgery. His principal research focus is on the cell and molecular biology of organ pre-conditioning and stress protein expression. Other research interests include the Kupffer cell, innate immunity, endotoxin handling and functional assessment of the liver in the context of surgery and transplantation. He is also involved in medical education and
distance learning.
I spent some time with Dr David Pier and Dr Paula Smith, who introduced me to the Edinburgh surgical online distance learning programme. David Pier is Academic eFacilitator for the ChM in General Surgery and the ChM in Trauma and Orthopaedics, two online postgraduate programmes delivered in partnership between the University of Edinburgh and the Royal College of Surgeons of Edinburgh. His background is in the basic sciences; he has a BSc degree in Biochemistry from the University of Edinburgh and a PhD in Cancer Cell Biology from the University of Leicester. Paula Smith is Academic eFacilitator for the MSc in Surgical Sciences and the ChM in Urology.
David took me through a tour of the online educational programmes, including visits to the interactive discussion groups that make the educational program a much more active and participatory experience than typical self-study programs. The course is case-based, and highly interactive. The distance learning programmes started in 2007 with the launch of the MSc in Surgical Sciences. A ChM degree in General Surgery was added in 2011, followed by ChM degrees in Urology, Trauma and Orthopedics in 2012, and ChM degrees in Vascular and Endovascular Surgery in 2013. The MSc in Surgical Sciences is now the largest Master’s program offered at the University of Edinburgh, with approximately 115 new students per year. The ChM programs have also grown considerably, with nearly 400 students from 40 countries, raising revenues of approximately £1million per year.
The distance learning programs were developed in response to a number of needs that arose due to changes in surgical training, the most important of which was the significant restrictions in duty hours for postgraduate medical trainees in the United Kingdom. Limited hours of service provide limited opportunities for trainees to gain experience with all of the problems likely to be encountered in surgery. The distance learning programmes provide another mechanism to ensure that trainees have achieved a core knowledge base by the end of their training. Trainees are evaluated on standardized examinations, and also are assessed based on participation in the discussion groups. Active participation of many of the surgeons at the University of Edinburgh has been a key factor in the success of this program.
Hi met with Damian Mole, Clinician Scientist, Clinical Senior Lecturer and Honorary Consultant Surgeon at RIE. Over lunch, we discussed his research interest in inflammation and immune modulation, particularly in pancreatitis. Using in vitro and small animal models of experimental acute pancreatitis, Damian is focusing on better understanding the inflammatory pathways, and identifying therapeutic targets.

My last meeting was with Andrew de Beaux. Andrew’s clinical practice focuses mainly on abdominal wall reconstruction, although he practised mainly foregut oncologic surgery earlier in his career. An amateur pilot, his office is covered with flight maps of Great Britain. We discussed surgical approaches for abdominal wall reconstruction, including component separation procedures, as well as composite tension free repairs with subfascial mesh. Andrew will be chairing the European Hernia Society’s 36th Annual International Congress in Edinburgh in May 2014.
The evening’s social event was dinner with Professors Garden and Wigmore and Damian Mole at Ondine Restaurant.
Western General Hospital
Specialty surgery is heavily regionalized in Scotland. The colorectal unit at the Western General Hospital is a unit of 13 surgeons, operating in up to 4 Operating Rooms on any given day. The colorectal division includes very successful researchers, such as Malcolm Dunlop, who had just learned he had been awarded a £5 million grant to continue his research on the genetics of colorectal cancer (while we were waiting for a cab to take me back to the airport).
In the morning I met Hugh Paterson, who accompanied me to the WGH multidisciplinary colorectal tumor board. I have attended many tumor boards, but I have never seen a tumor board like this one. First, it was fully attended by all the appropriate specialties: colorectal surgery, medical oncology, radiation oncology, pathology, diagnostic radiology, oncology nurses, and a tumor board coordinator. I counted 30 people in the room at one point. Second, we reviewed nearly 50 cases in 90 minutes—the radiologist was familiar with all the films (CT, MR, PET), and highlighted findings in a rapid-fire staccato. Third, they were highly organized. The tumor board coordinator had prepared summaries of all the cases with key information, and there was a printed guide to all the cases. Fourth, there was a videoconference link to other participating sites, and the telecommunications worked seamlessly.
The Division of General Surgery at WGH is really a colorectal surgery unit. The GPs and paramedics in Edinburgh and environs seem to really understand the division of surgical focus between the Royal Infirmary of Edinburgh and WGH; apparently all cases that seem like lower GI surgical problems are sent to WGH and all cases that seem like upper GI surgical problems go to RIE. Exactly how the GPs and paramedics can distinguish lower and upper GI surgical emergencies remains a mystery to me; our ER physicians and housestaff in fully equipped emergency departments sometimes get this wrong, and that’s with the benefit of CT scans. In any case, everything "from the duodenum down" goes to WGH, and everything else goes to RIE.
Because 90% of all care in Scotland is insured through the NHS, there appears to be little competition among surgeons for patients, and very little private surgery. That, in addition to its distributed geography and relatively small population of 5 million, has allowed Scotland to regionalize surgical services on an impressive scale, and without the turf warfare and acrimony you might expect.
Adelaide

My host in Adelaide was Guy Maddern. He picked me up at the airport on my arrival, and he and Liliane graciously hosted me at their lovely home. I was provided with excellent accommodations in the guest room. The house was otherwise quite a bustling affair, housing Guy and Liliane’s children, a dog and three cats. I was hosted to a family dinner at the Maddern residence on my arrival.
This is quite an interesting time for surgery in Adelaide. The two major hospitals (Royal Adelaide and the Queen Elizabeth Hospital) are in the process of administrative merger, and Guy in instrumental in this administrative change. An enormous brand new hospital rising in Adelaide’s Central Business District is visible from the airplane as it approaches the Adelaide airport.
In the morning, Harsh Kanhere picked me up and drove me to the department of surgery at the Queen Elizabeth Hospital. I presented a talk entitled "What can be learned from non-randomised studies of surgical procedures?" I didn’t realize that Peter Hewett, lead author of one of the major articles I reviewed in my presentation (the "Australasian Randomized Clinical Study Comparing Laparoscopic and Conventional Open Surgical Treatments for Colon Cancer") would be present. Luckily, it was favorably reviewed in my talk, avoiding any awkward explanations to my host audience. The talk was well received, and I fielded several thoughtful questions for the assembled audience.

Following my lecture I joined a clinical governance meeting chaired by Guy. As I came to learn, Guy is integrally involved in almost all aspects of surgery in Adelaide. This particular meeting included a variety of people representing the Department of Surgery at the Queen Elizabeth hospital, including nurses and administrative leaders. A number of clinical issues were reviewed, including problems such as record-keeping by a physician whose handwriting was difficult to read, and where cataracts procedures should be done, particularly in light of the impending administrative changes in the Adelaide hospitals.
Mau Wee, a research resident, took me on a tour of the Basil Hetzel Institute (BHI) for Translational Health Research. Mau is originally from Malaysia, and is currently conducting research on liver reperfusion. Guy is his research supervisor. The BHI institute is a brand-new, state-of-the-art research building on the main campus area of the Queen Elizabeth Hospital. It has facilities for clinical trials and clinical research, as well as dry-lab carrel space, and wet labs. Over coffee, Mau explained his career pathway, including the residency training system in Australia.
I met with Guilherme Pena, a research fellow from Brazil who also works at the Royal Australasian College of Surgeons in simulation research (more about this below) and who will be joining the department as a clinical surgery resident next year, and Markus Trochsler, a young faculty member from Switzerland. They presented some of their research on the use of chitosan-dextran gel for use in adhesion prevention. Although I am familiar with some of the research on mechanical and chemical means of prevention of peritoneal adhesions, I had never heard of chitosan-dextran gel. It has been used in clinical applications by ENT surgeons for prevention of adhesions after nasal sinus surgery. Based on this success in human clinical use, Guilherme and Markus were tasked with conducting animal studies to explore its use in the peritoneal cavity.
They conducted a variety of experiments in rats and pigs. The pig experiments were most interesting, and it appears that the major problem at this point is the toxicity of chitosan-dextran gel in large animals. The first task was to create a pig model of severe adhesions, which they accomplished by a combination of peritonectomy and bowel suture. In initial studies, the pigs developed severe complications (bowel obstruction, perforation) due to the weight of crystallized material from the gel. To modify the delivery system, the concentration of the solution was changed. Currently, they seem to be noticing severe allergic reactions (desquamative skin eruptions) in the pigs after instillation of gel in the peritoneal cavity. The work continues.
I then met Guy at the Royal Australasian College of Surgeons building in Adelaide, where I spent the rest of the day. I toured the College buildings, including a beautiful old mansion which the College owns and uses for meetings and events, and another premises that the College rents for its working offices. The main headquarters of the Royal Australasian College of Surgeons is in Melbourne; I would visit that building 2 days later. The College has a number of Divisions. The Division of Research, Audit and Academic Practice, has a number of activities that Guy leads. These areas of concentration includes: Academic Surgery, ASERNIP-S, Morbidity Audits (such as the breast cancer audit), Mortality Audits, Project Office, and Scholarships).
One general theme of my James IV travels was a much better understanding of the structure of surgical organizations in the English-speaking world, particularly with respect to the role of universities, hospitals, and "Colleges" (which serve as one or more of: professional organization, self-regulatory organization, educational authority for residency training, assessment of competency, provider of licensure for surgical practice, provider and accreditor of continuing medical education for practicing surgeons, research funding organization, technology assessment authority, and consultant to government). The Royal Australasian College of Surgeons, which has authoritative jurisdiction over surgeons in Australia and New Zealand, is among the most active and influential Colleges that I encountered.
Guy leads a division of the College called ASERNIP-S (The Australian Safety & Efficacy Register of New Interventional Procedures – Surgical). This is a large technology assessment body, operated by a number of clinical epidemiologists who do the actual work of conducting systematic reviews, appraising evidence, and providing guidance. The agency that has authority for approval of new health products in Australia is the TGA. There is a body called MSAC, which advises governments about coverage of new health technologies (similar to the Ontario Health Technology Advisory Committee [OHTAC], where I was a member for several years).
The Division of Research, Audit and Academic Practice also conducts a number of other interesting activities. They are quite interested in non-technical skills in surgery, and I viewed a presentation fo simulation-based research looking at non-technical skills (communication, situation awareness) among surgical trainees using a tool called NOTTS. I also toured the simulation laboratory at the College building. They have two mobile simulation laboratories.
I then attended conference calls related to the Australian and New Zealand Audit of Surgical Mortality meeting. The audit is a really interesting initiative. The conference call was attended by regional heads of all the Australian states. The College requires mandatory reporting of all deaths in an Australian hospital when care was provided by a surgeon. Reports go through an initial screening and a secondary review by a peer reviewer. Peer review activity is compensated, and all information is protected by law. Participation in the audit is required for the College to provide CME attestation. There is incredible buy- in to the concept of the audit, and this is a hugely successful program. The audit does not just serve a quality assessment and quality improvement role, but also is a valuable source of research data, (one of the first articles related to the audit was just accepted in Annals of Surgery while I was in Adelaide).
I had dinner with surgeons of the upper GI unit (and spouses) in the Lion Hotel. My next day in Adelaide was not as full. Liliane took me on a driving tour of the city and to the beach for lunch. I then went back to the Queen Elizabeth Hospital, where I presented medical grand rounds entitled "Introduction of Surgical Safety Checklists in Ontario, Canada: Effectiveness in the real world". Frank Bridgewater gave me a reprint of an article authored by him, Guy, and Glyn Jamieson, on problems with the Angelchik prosthesis. We had discussion at dinner about problems with the surgical literature, and how the literature has a lot of material on the benefits of new technology but not much about problems with technology. I hadn’t realized there was published literature on complications due to the Angelchik prosthesis.
Melbourne
My visit in Melbourne was coordinated by Robert Tasevski, an endocrine surgeon who was a graduate student with me in clinical epidemiology while he completed a surgical oncology fellowship at the University of Toronto. I spent my first night in Melbourne catching up with Rob, and exploring beautiful central Melbourne, one of the most beautiful and functional cities I have ever visited.

I spent a morning in the clinical offices of Wendy Brown, President of the Obesity Surgical Society of Australia and New Zealand, and Director for the Centre for Obesity Research and Education (CORE) at the Glen Iris Private Surgical Hospital. The Glen Iris Private Surgical Hospital is a small private hospital in suburban Melbourne, which provides a variety of surgical services, including laparoscopic adjustable gastric bands. As a surgeon practicing bariatric surgery—principally laparoscopic Roux en Y gastric bypass—and with little experience with gastric bands, I was very interested in how patients are evaluated and followed up.
The morning was very informative and enlightening for me.
Laparoscopic adjustable gastric bands are the mainstay of obesity surgery in Australia, which is a very different practice than our approach in Toronto, as well as in many other centres. I observed how closely and carefully the gastric band patients were followed, and  came to appreciate the intensity of follow up that is required for a successful laparoscopic gastric band program. When I asked Wendy why so many bariatric procedures in Australia are gastric band placements, she explained that this was really a response to patient preference and demand. My observations in the clinic corroborated this; the Australian patients seemed very much against gastric bypass and other "permanent" and "invasive" procedures. There is a big social and cultural difference
between Australian and North American patients who seek obesity surgery. Patients are followed incredibly closely, with multiple appointments and band adjustments. I learned that band adjustments are titrated to the patients’ perception of satiety/hunger, not dysphagia.
came to appreciate the intensity of follow up that is required for a successful laparoscopic gastric band program. When I asked Wendy why so many bariatric procedures in Australia are gastric band placements, she explained that this was really a response to patient preference and demand. My observations in the clinic corroborated this; the Australian patients seemed very much against gastric bypass and other "permanent" and "invasive" procedures. There is a big social and cultural difference
between Australian and North American patients who seek obesity surgery. Patients are followed incredibly closely, with multiple appointments and band adjustments. I learned that band adjustments are titrated to the patients’ perception of satiety/hunger, not dysphagia.
I met with Professor Jim Bishop AO, Executive Director of Victorian Comprehensive Cancer Centre (VCCC). There are major changes underway regarding cancer care in Melbourne, with development of a new multidisciplinary cancer centre. Prof. Bishop was very much interested in our experience with Cancer Care Ontario, in particular our experience with population-based cancer-related health services research. To this end, I was able to shed quite a bit of light on our activities, in my capacity as head of the cancer research program at the Institute for Clinical Evaluative Sciences (ICES), in Ontario Canada. Prof. Bishop was well-informed about the structure of Cancer Care Ontario, and had many several trips to Canada. He asked about our experience with quality reporting (particularly the Cancer System Quality Index, or CSQI) and our various publications, including an atlas of cancer surgery that I edited in 2008.

I spent some time in the busy general surgery clinic of the Royal Melbourne Hospital with Julie Miller, a general surgeon who emigrated from the US who focuses on endocrine surgery. I saw several patients in the clinic with her and the trainees, and was impressed once again at how similar our patient problems are around the world, and particularly the difficult patient problems. We saw a patient with chronic abdominal pain who had undergone multiple previous laparotomies, with no obvious explanation for pain, but who was agitating for another laparotomy. I spent some time with the chief resident discussing some communication strategies for what we all thought would be a difficult patient encounter. I saw a patient with Julie who had a multinodular goiter with a dominant nodule, who presented to the clinic with no previous documentation or records. Julie had suggested a biopsy. The patient thought she already had one. This led to a (familiar to me) series of searches and calls to the family doctor to try to divine what tests and procedures the patient had already undergone.
I met with Bruce Mann, a previous James IV Travelling Fellow, and Head of Royal Melbourne Hospital & Royal Women’s Hospital Breast Service. Bruce was very helpful in coordinating my visit, and giving me helpful context on the practice of general surgery and hospital care in Melbourne. Bruce is also steeped in the knowledge of surgical history, and the James IV program in particular. Here I understood the value of a fellowship of surgeons who have been James IV travelers, who share a unique experience that only fellow travelers can relate to.
Bruce and I met with Dr Gareth Goodier, recently appointed Chief Executive of Melbourne Health. It quickly became evident to me that the main objective of the hospital was the implementation of an electronic patient record. I saw from my experience with Julie in the busy general surgery clinic that RMH had no electronic medical record system. The patient with chronic abdominal pain, for example, had a record consisting of several thick file folders comprising multiple hospitalizations, the earliest of which were archived and effectively inaccessible. I quickly understood that Gareth had been hired in large measure because he had recently introduced an EMR in Cambridge UK, where he had previously been a hospital executive. He asked many questions about our EPR at my hospital (Quadramed, as it turns out, although we were in the process of evaluating bids for a new EPR vendor).
I had a lovely dinner at the Flower Drum Restaurant in Melbourne, a very authentic Chinese restaurant. Bruce Mann and I were joined by other James IV fellows, including Julian Smith, and Donald "Scottie" Macleish. Scottie was a retired vascular surgeon, who is remarkably sharp and active for his years. He asked me about various colleagues of his in Toronto, none of whom I knew, expect for the ones who had lectures named after them. We shared wonderful food, conversation, and friendship. After dinner we walked to the Royal Australasian College Building, beautifully illuminated in the night, where Scottie gave me a lift back to my hotel.
I had an early morning the next day, leading a teaching session with the general surgery registrars on adrenal diseases, one of my clinical interests. The registrars were knowledgeable, attentive, and very appreciative for the opportunity of hosting a visitor. After my teaching session, I had breakfast with Rose Shakerian, General Surgeon and Research Fellow. Rose’s work focused on evaluation of a new acute care surgery service at RMH. I gave her my thoughts on how she could implement her study, which relied principally on detailed data from an existing database used to manage the acute care surgery service.
My last meeting in Melbourne before heading off to Sydney was with Prof. Danny Liew, Director of the Melbourne EpiCentre. This is a hospital-based epidemiologic research unit. The unit seemed to have all the right people—methodologists, statisticians, economists—and focused mostly on chronic disease research. What was missing was collaboration with clinical researchers, who could really benefit from the technical and methodologic expertise of the EpiCentre. This reinforced to me the importance of ensuring that research units are closely allied with the people who can best use their resources.
I wished Rob Tasevski farewell and expressed my sincere thanks, and headed off to Sydney.
Sydney
My visit to the Royal Prince Alfred Hospital and Professor Michael Solomon’s research unit (SOuRCe, Surgical Outcomes Research Centre) began in the morning when I met with Cherry Koh, a colorectal surgeon at the Royal Prince Alfred. Cherry took me on tour of the various hospital buildings, including the new cancer centre (The Chris O’Brien Cancer Institute). It was interesting to see this new cancer centre building, an entirely new construction, with new structures for oncology clinics and multidisciplinary teams. Cherry told me the story of Chris O’Brien, a popular Australian head and neck cancer surgeon who tragically died from glioblastoma multiforme in 2009. He had developed a proposal to transform the Sydney Cancer Centre into a modern comprehensive cancer centre, and raised funds from the Australian Government and philanthropic donors. The cancer centre will focus on patient centered care.
After seeing the new Melbourne and Syndey cancer centres, I realized how fractured cancer care is in many places around the world. The concept of comprehensive cancer centres, while popular in the United States and Canada, was a relatively new concept in Australia. The intent of the cancer centres is to integrate all the cancer care disciplines, to provide multidisciplinary and comprehensive care.

Cherry also explained the history of the Royal Prince Alfred hospital. Prince Alfred, the son of Queen Victoria and Albert, was injured during an assassination attempt while visiting Sydney. He was treated at a hospital staffed by nurses trained by Florence Nightingale, and following his recovery, a public campaign to raise funds for a new hospital building was enacted by the people of Sydney to commemorate to survival of the prince.
I was very much interested in visiting the Surgical Outcomes Research Centre. I had first met Michael Solomon in the early 1990’s when he was a clinical fellow in colorectal surgery at Mount Sinai Hospital in Toronto, and where I was a clinical clerk in general surgery. Professor Solomon completed clinical epidemiology training with Robin McLeod, and had initiated a very productive and successful clinical research unit focused on clinical epidemiology.
I first met with Professor Jane Young, an epidemiologist focusing on cancer epidemiology who collaborates closely with Prof. Solomon. I then attended a SOuRCe Director’s meeting. Once again, it was interesting for me to see how leaders of clinical research units run their research operations. I learned about the funding of SOuRCe, and the challenges associated with ensuring continuing funding of a research unit. Prof. Solomon took me on a tour of the colorectral unit and research areas.

I presented my talk—"What can be learned from non-randomsied studies of surgical procedures?"—to an interested group of researchers and clinical trainees. It was interesting to present this research to this particular group, since there was considerable overlap between the focus of my presentation and the work of SOuRCe. In fact, I cited several articles authored by Prof. Solomon, stemming both from his original work when he was in Toronto, as well as more recent work his group has done on the analysis of studies comparing laparoscopic and open colon surgery.
I had lunch with Cherry Koh at a Vietnamese restaurant in New Town, not far from the Royal Prince Alfred. She then took me on a tour of the beautiful campus of the University of Sydney, with its quadrangle and college buildings modeled after Cambridge.
Hong Kong

My visit to Hong Kong was a highlight of my travels. I had never visited East Asia, and the opportunity to explore a different environment and culture was very exciting. I visited the Department of Surgery of the Li Ka Shing Faculty of Medicine, University of Hong Kong. My visit was based mainly at the Queen Mary Hospital in Hong Kong.
When I arrived, I met with Gloria Wong for introductions and formalities. Gloria was an administrative assistant to the Department of Surgery. By coincidence, Gloria had lived in Toronto some years ago, and we talked about the neighbourhoods where she had lived, and how the city had changed. I was presented with generous gifts upon my arrival, including a University of Hong Kong necktie, which I wore during my visit in addition to my James IV tie.
I then met with Professor James Wong, the well-known emeritus chair of the Department. We discussed some of the recent changes in the Department of Surgery at Queen Mary Hospital, as well as some of the opportunities that arose due to the opening up of China to partnerships with Hong Kong in health care. Prof. Wong asked me about acquaintances back in Toronto, including Dr. Bernard Langer, an accomplished academic surgeon and surgical leader in Toronto who was well-recognized around the world for his accomplishments in academic surgery.
I met with Simon Law, an upper gastrointestinal surgeon, and had the opportunity to observe him in the operating room as he performed a laparoscopic gastrectomy.
 Watching the surgical technique of the surgeons at Queen Mary hospital was truly fascinating. I could see a clear difference
in the approach to surgery from typical North American settings.
The surgeons at Queen Mary were absolutely meticulous and
precise, focused on clear anatomic planes, and operated in a field that was always bloodless. Surgeons
would use a variety of hemostatic techniques—ultrasonic dissection, bipolar electrocautery, monopolar instruments—often in succession, and with the effect that I never observed a single drop of blood in the operative field. Vessels were always anticipated, identified, and precisely ligated. This made for operative procedures that were an absolute pleasure to observe.
Watching the surgical technique of the surgeons at Queen Mary hospital was truly fascinating. I could see a clear difference
in the approach to surgery from typical North American settings.
The surgeons at Queen Mary were absolutely meticulous and
precise, focused on clear anatomic planes, and operated in a field that was always bloodless. Surgeons
would use a variety of hemostatic techniques—ultrasonic dissection, bipolar electrocautery, monopolar instruments—often in succession, and with the effect that I never observed a single drop of blood in the operative field. Vessels were always anticipated, identified, and precisely ligated. This made for operative procedures that were an absolute pleasure to observe.
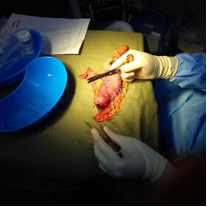
After the specimen was resected, Prof. Law took the specimen to a back table, where he identified lymph nodes at various stations, dissected them out, labelled them, and sent them separately for pathologic evaluation. The care and attention paid to anatomic staging of lymph nodes was unprecedented in my experience.
I then met with Chung-Mau Lo, Chin Lan-Hong Professor and Chair of Hepatobiliary and Pancreatic Surgery, and Head, Department of Surgery at The University of Hong Kong. We had an interesting conversation about the issues in the Department of Surgery, as well as the new opportunities presented by the opening of China to collaboration in health care. The University of Hong Kong had just started a new collaboration with a new hospital in Shenzhen in mainland China. Surgeons from the University of Hong Kong were travelling to Shenzhen to perform surgical procedures and staff clinics.

I had dinner with James IV fellows at the Shun Fung Restaurant, American Club, atop a skyscraper in central Hong Kong, overlooking the harbour and Kowloon. The main topic of discussion was the different health systems in different countries, their strengths and weaknesses, and how they influence the culture of medical practice. Interestingly, local news from Toronto—in this case, the ongoing saga of the wayward mayor of the City of Toronto, Rob Ford—had reached Hong Kong, and I was asked about our municipal politics as well!
The next morning I attended a clinical case conference attended by the entire Department of Surgery. The first case was presented by the plastic surgeons, a case of Ewing sarcoma involving the chest wall. The second case presented was that of a patient with an obstructing left sided colon cancer in the presence of cirrhosis and a hepatic mass. The patient, a prisoner, was present in the front of the conference room, available for examination. The imaging was reviewed, and I was asked for my clinical opinion. Not being a hepatic surgeon, I dug deep into my knowledge of the radiologic appearance of hepatocellular carcinoma, and based on the peripheral enhancement of the lesion on the contrast scan, I proposed that the hepatic mass was likely a hepatocellular carcinoma arising in the setting of cirrhosis, perhaps unrelated to the newly apparent obstructing colonic mass.
examination. The imaging was reviewed, and I was asked for my clinical opinion. Not being a hepatic surgeon, I dug deep into my knowledge of the radiologic appearance of hepatocellular carcinoma, and based on the peripheral enhancement of the lesion on the contrast scan, I proposed that the hepatic mass was likely a hepatocellular carcinoma arising in the setting of cirrhosis, perhaps unrelated to the newly apparent obstructing colonic mass.
After the case conference, I was met by CC Foo, who took me to breakfast and tour of the hospital and research facilities.
We travelled to the nearby laboratory facilities of Department of Surgery at Li Ka Shing Faculty of Medicine, where Dr. K. Man presented her laboratory work.
I had lunch with Jensen Poon and CC Foo and a sushi restaurant not far from my hotel. After lunch, I had another opportunity to observe surgery at the Queen Mary hospital, this time a laparoscopic subtotal  colectomy, performed by Wai Lun Law, Anthony Cheung and Anne Cheung Professor in Innovative and Minimally Invasive Surgery, Chief of the Division of Colorectal Surgery, and director of the Surgical Skills Centre. The patient was a young man with attenuated polyposis and multiple colonic tumors. Once again, I was fascinated by the meticulous and completely hemostatic approach towards gastrointestinal surgery.
colectomy, performed by Wai Lun Law, Anthony Cheung and Anne Cheung Professor in Innovative and Minimally Invasive Surgery, Chief of the Division of Colorectal Surgery, and director of the Surgical Skills Centre. The patient was a young man with attenuated polyposis and multiple colonic tumors. Once again, I was fascinated by the meticulous and completely hemostatic approach towards gastrointestinal surgery.
That evening, I presented my lecture "What Can Be Learned From Non-randomised Studies of Surgical Procedures?" Once again, the audience was very receptive, and asked many insightful questions. After my lecture, I was hosted to another wonderful dinner with a number of faculty and trainee surgeons. We were joined by Siu-Yin Chan, an upper GI surgeon who arrived late because she had been operating in Shenzhen all day.
Amsterdam VUMC
I had a wonderful time in Amsterdam, which included one of the worst hurricanes in recent years (which I somehow slept through due to jet lag), as well as visits to major art galleries, including the Rijksmuseum, Van Gogh museum and Anne Frank House. My itinerary at VUMC (Free University Medical Centre) included a number of academic events.
Professor Jaap Bonjer was my host in Amsterdam. He was recruited to Dalhousie University in Halifax, NS in 2004 from Erasmus University in Rotterdam, where he had a stellar career as an academic surgeon and trialist, coordinating landmark multicentre surgical trials such as the COLOR trial comparing laparoscopic vs open colon cancer surgery. He left Halifax in 2009 to take on the job of Head of the Department of Surgery and Chairman at VUMC, where he has nurtured an outstanding Department of Surgery.
I began my days with the surgical team’s clinical conference at 07:45. There were several surprising things about how the surgical department at VUMC functioned. First, the scope of the Department of Surgery is quite different from what we consider the scope of general surgery practice in North America. In the Netherlands, general surgeons call themselves "surgeons" rather than "general surgeons". Their scope of clinical activities includes what we consider "general surgery" in North America (gastrointestinal surgery, surgical oncology, trauma, endocrine), but also includes much of emergency orthopedics (fracture management, including both closed reductions as well open reductions with internal fixations of extremity fractures, hip fractures, and spinal fractures except cervical spine fractures). The surgeons also perform vascular surgery (emergency and elective).
The second surprising aspect of how surgical care was organized was the comprehensive team approach. Rather than organization of surgical teams around specific staff or clinical programs, the entire team worked together as a truly integrated team. In the morning, the entire team (staff surgeons, residents, students) reviewed the cases admitted overnight, as well as the OR cases planned for the day. These rounds served simultaneously as a morbidity and mortality conference as well as a "business" meeting, during which the clinical activities of the day were planned and staffed. Although it was carried out in Dutch, I was able to follow the cases. Typical of Amsterdam, where so much transportation is by bicycle, one unfortunate case was reviewed of a young girl who was thrown from her bicycle during a collision with a bus. She sustained a contained disruption of her aortic arch, and presented to the ER stable with a wide mediastinum. Unfortunately, she became unstable during attempts to stent the aortic disruption, and emergency laparotomy and repair of the aortic tear was not successful in rescuing her.
I toured the Emergency Department at VUMC. The trauma system in Amsterdam differs from typical North American trauma teams, in that the transport trauma team includes a trauma surgeon, nurse and anesthetist who travel to the field for serious injuries. They could travel by helicopter or emergency response vehicle (not an ambulance equipped for transporting patients, but a vehicle able to navigate streets, with appropriate resuscitation equipment for field trauma interventions).
There were several postoperative care units that I toured in VUMC. One of these was an acute care unit; an inpatient unit intended for 48 hour stays. This unique hospital ward housed patients from a variety of services (surgery, internal medicine). Patients who could not be discharged within 48 hours were transferred to an appropriate destination unit within 48 hours. Most acute care surgical cases (appendicitis, cholecystitis) were discharged within the 48 hour period, making this unit a very sensible way to take pressure off the other hospital wards.
I joined the resident team for their clinical ward rounds. Residents in Europe are limited to a 48 hour work week, which in practice is quite a different work week than our residents are used to. For example, if a resident takes call on a Saturday, they are entitled to a lieu day off during the subsequent week. On call shifts for a day end at 10:00 P.M., with a new team replacing the resident who has taken call from 08:00 to 22:00. Rounds were attended by typical teams of surgical trainees and students.
I attended the ORs in VUMC. These were state of the art operating rooms, with full MIS functionality, as well as surgical robots (rarely used by the general surgeons). I spent much of one day observing a Whipple procedure.
I attended multidisciplinary endocrine oncology rounds. These rounds are typically attended by surgeons, endocrinologists, pathologists, and radiology. Several cases were presented, including a case of Cushing’s syndrome caused by multinodular adrenal hyperplasia (so called "AIMAH", or ACTH- independent multinodular adrenal hyperplasia). I was asked how we manage these patients in Canada. The answer to the question was somewhat complex, since there is an active endocrine oncology unit in Montreal championed by Andre Lacroix, that investigates these patients aggressively, looking for endocrine responses to vasopressin, mixed meal, etc, and tailors treatment according to the specific endocrine receptor defect. In Toronto, we would typically resect one or both adrenal glands. Practice in Amsterdam was similar to our practice in Toronto. We reviewed the case of a bipolar patient on lithium with hypercalcemia and increased PTH who had twice been scheduled for parathyroidectomy (and who had then twice been cancelled due to a normal calcium level on the day before surgery). We decided to cancel her third booked surgery (scheduled for the next day!).
I spent some time with Professor Bonjer in his surgical outpatient clinic. It was somewhat reassuring to see that the vexing problems we face in academic surgical practice are quite similar in North America and Europe. In addition to the straightforward (inguinal hernia), we saw cases of chronic pain after ventral hernia repair (the Dutch appear to have solutions no better than our own; reassurance, setting expectations, encouraging non-pharmacological approaches [although Jaap seemed somewhat dubious of my suggestion of meditation, yoga or aerobic exercise], and non-narcotic pharmacologic approaches such as neuromodulator medications. We saw a complex patient who had been recovering in rehab from a stroke with a soft tissue lump in her lateral thigh. Not sure if this was lipodystrophy, fat necrosis, or a soft tissue neoplasm, we decided to send her for an MRI scan. Thankfully the patient with the inguinal hernia agreed to have surgery the next day, replacing a case for the bipolar patent on lithium whose parathyroid exploration had just been cancelled.
I meet with several PhD students at VUMC. Most of the students have clinical backgrounds, typically they have completed medical school and are either awaiting positions for academic residencies (residency training positions intended to achieve specialty training as a consultant) or medical school graduates hopeful of a surgical training position, but who are pursuing non-academic residencies (hospitalist or assistant physician positions) in the meantime. Most of these students’ projects were multicentered randomized controlled trials related to surgery. Students reviewed protocols for a study of selective decontamination of the digestive tract (SDD) prior to colorectal cancer surgery, as well as study of a laparoscopic vs open surgery for ventral hernia, and the COLOR-2 trial comparing laparoscopic and open surgery for rectal cancer.
I learned quite a bit about how the Europeans have been so successful at conducting surgical RCTs, at least in comparison with us North Americans (including the cooperative oncology study groups). The success of the Europeans has a lot to do with culture. Surgeons are enthusiastic participants in RCTs, enrolling patients, collecting data, and providing the data back to a central study coordinating centre without subject finding fees or other grants. Investigators are invited to annual or bi-annual investigators meetings. The central coordinating groups pay for their travel, housing and subsistence, and the meetings serve as key opportunities for academic linkage, exchange, and professional development of the participating surgeons. As a result, the large European surgical trials are run on a virtual shoestring. Typically the trials are overseen by one or two graduate students, with support of a statistician and database manager. Financial support may come from an industry grant, university grants, or academic funds from activities such as CME courses. The ability to enroll multiple sites and surgeons (for example, the COLOR 2 trial had 30 participating sites, none within the United States), has much to do with culture and engagement. It was an eye opener into what is possible when surgeons share a common interest in finding answers to the major questions that face us on a daily basis.
I gave a presentation to the VUMC Department of Surgery entitled "What can be learned from non- randomised studies of surgical procedures?" The lecture was well-received and participants asked many thoughtful questions. I must say it was somewhat awkward delivering a lecture that focused on all of the (insurmountable?) problems facing attempts to conduct RCTs of surgical procedures, in a department of surgery that is arguably the most successful coordinating centre of surgical RCTs in the world!
Israel

In Israel, I visited the Hadassah Ein Kerem Medical Center in Jerusalem. There are two campuses of Hadassah Medical Center, on in Ein Kerem and one at the Hebrew University campus at Mount Scopus. Most of the activity in general surgery is at the Ein Kerem Campus. My host for the visit was Dr. Yoav Mintz, an MIS surgeon. I met with several surgeons, including Professor Aviram Nissan, head of the Department of Surgery at Hadassah. Professor Nissan is a surgical oncologist. I also met with Professor Avi Rivkind, Chair of the Department of Surgery, and an internationally recognized expert in trauma.
Dr. Mahmoud Abu Gazala, an associate surgeon in the department, met me in the morning and helped show me around the hospital. I gave a talk at the Department of Surgery morning rounds, entitled "Introduction of Surgical Safety Checklists in Canadian Hospitals". I gave the talk in English, and I felt quite comfortable that it was understandable to all the attendees.
Following my lecture, I attended surgical academic rounds. One of the residents presented a case of dysphagia occurring several years after a laparosco pic Nissen fundoplic ation. The case
slides were presented in English—for my benefit—but the discussion was in Hebrew. I was able to follow
dysphagia occurring several years after a laparosco pic Nissen fundoplic ation. The case
slides were presented in English—for my benefit—but the discussion was in Hebrew. I was able to follow
 With Professor Avi Rivkind, Chair of the Deaprtment of Surgery, Hebrew University
much of the discussion, and when asked for my opinion I thought I was able to provide a reasonable approach to investigation and management.
With Professor Avi Rivkind, Chair of the Deaprtment of Surgery, Hebrew University
much of the discussion, and when asked for my opinion I thought I was able to provide a reasonable approach to investigation and management.

After my lecture, Yoav led me on a tour of the hospital. He described several innovations in surgical practice, including a technique he has developed for laparoscopic sleeve gastrectomy in which he removes the excised portion of the gastric fundus through a gastrotomy. The hospital itself was huge. I visited famous parts of the hospital, including the famous Chagall stained glass windows, as well as Albert Einstein’s Nobel Prize, both of which are housed in the Medical Center.
I toured the construction of new operating rooms in the hospital. The current operating rooms are quite old, having been built in the 1970’s. Due to government mandate, certain areas of the hospital (including the operating rooms) must be resistant to chemical, biological and nuclear war. As a result, the new operating rooms are being constructed four stories below the basement, in reinforced concrete bunkers with thick concrete walls. Although the result is a very stark, quite, and "industrial" environment, the project crew in charge of constructing these new ORs seemed very aware of the need to keep them personal and comforting, including a lot of outside images in the artwork, for example.
Overview/synthesis
Throughout my travels, which took me to a number of continents, countries, cultures and health systems, I identified a few themes which I thought were of note, and warranted further reflection.
The role of the professional colleges
During my training and professional career, I had developed the misunderstanding that the entities that license, regulate and educate surgeons were more or less similar. In Ontario, Canada, for example, the College of Physicians and Surgeons of Ontario (CPSO) serves as a self-regulating body for the practice of medicine that protects and serves the public interest, by serving certificates of registration to physicians and investigating public complaints. The Royal College of Physicians and Surgeons of Canada (RCPSC) performs a variety of activities to strengthen the practice of specialty medicine and surgery, such as accreditation of residency programs, verification of requirements for certification of specialist physicians, conducts certification examinations, maintains certification of specialist physicians through continuing medical education programs, and a variety of other policy, advocacy, and educational activities. I had assumed that the regulation and support of surgical practice throughout the world had a similar structure; in the United States, for example, the American College of Surgeons and American Board of Surgery together have a similar mandate to the RCPSC, and the state licensing authorities provide functions similar to our CPSO.
What I discovered, though, is a large variation and richness in the different approaches for certification, regulation, discipline and education of surgeons and specialist physicians. Some Colleges have a long, rich history and are very innovative in serving the needs of practising surgeons and trainees, such as the Royal College of Surgeons of Edinburgh. Some are expansive, and serve as the only major entity with responsibility for governance and education of surgeons, such as the Royal Australasian College of Surgeons. Some of these Colleges found themselves in conflict between serving both the needs of trainees and practising surgeons. In each case, the development of these regulatory, investigative and educational entities served the local needs of the surgeons and the public, and appeared to fit within the culture of practice of the geographic region where it developed.
Attributes of successful surgical leaders
In my travels, I had the opportunity to interact with many contemporary luminaries in academic surgery. I was continually surprised at how welcoming they were to me as hosts, how much time they took to make my visit so enjoyable, and how much personal interest they took in me. I did note a few attributes of effective surgical leaders. First, none seemed to develop their authority through power, intimidation, or autocracy. Rather, they all were interested people, good listeners and communicators, ran meetings efficiently but always asking people—by name—for their input. They appeared to earn the loyalty and support of others by genuine interest in the common cause and by a personal commitment to development and excellence of the larger interest rather than any personal gain. Second, they all had original and innovative visions for development in surgery; ideas that were "disruptive" more than "incremental". Just a few examples would include Professor the Lord Ara Darzi and technological innovation in minimally invasive surgery; Professor O. James Garden’s innovations in trainee education; and Professor Guy Maddern’s innovations in technology assessment and clinical audit. A compelling original idea, and an energetic and passionate vision to carry it out, appears to be a pre-requisite for creating something spectacular. Third, they all found creative means to support their activities. Recognizing the limitations of typical sources of material support (hospitals, universities, funding agencies), these leaders found opportunities in unexpected places: governments, foundations, philanthropic donors, colleges, and subscription services, to name a few. Finally, they all served as role models, and had strong credibility as clinical surgeons. The most important constituency to win in establishing a position of leadership is that of your peer surgeons, and that will come only to those who are viewed as clinical leaders in our work as surgeons.
Succession planning
A related concept to that described above regarding the attributes of successful people is the issue of long-term sustainability of their signature programs, and succession planning. Successful academic surgeons are very busy people, tend to be very hands-on, and are frequently the singular creative spirit and driving force behind their programs. In many instances, the academic programs were hard to summarize succinctly; they were more a physical realization of a surgeon’s imagination rather than a conventional research unit. However, the very uniqueness, complexity, and category-defying nature of these units pose a major challenge to their long-term sustainability. In many instances, day-to-day management, and occasionally a strategic creative voice, was delegated to a program manager (often a protègè or PhD scientist). However, it was difficult for me to imagine many of these programs continuing in their established creativity and impact after the departure of the surgical leader. Tellingly, none of the programs I visited were "inherited" from somebody else. I asked some of the surgical leaders about this; many acknowledged that the issue of succession planning and long-term sustainability after their departure was not something they had an explicit plan for. I imagine that in many cases, programs will be broken up, with some of the components taken up by junior partners or scientific leads, while the remaining parts of the program many disappear. What became very clear to me was the importance of building effective layers of leadership within a program, and delegating important creative aspects to junior people where possible.
Conclusion
My experience as a James IV travelling fellow was the highlight of my professional career. I learned a lifetime of lessons about the world, about people, about programs, and about building a vibrant and creative future for academic surgery. I am grateful to the James IV Association of Surgeons for providing me with this opportunity. I will carry these insights and lessons with me for life.
Sincerely, David R Urbach MD